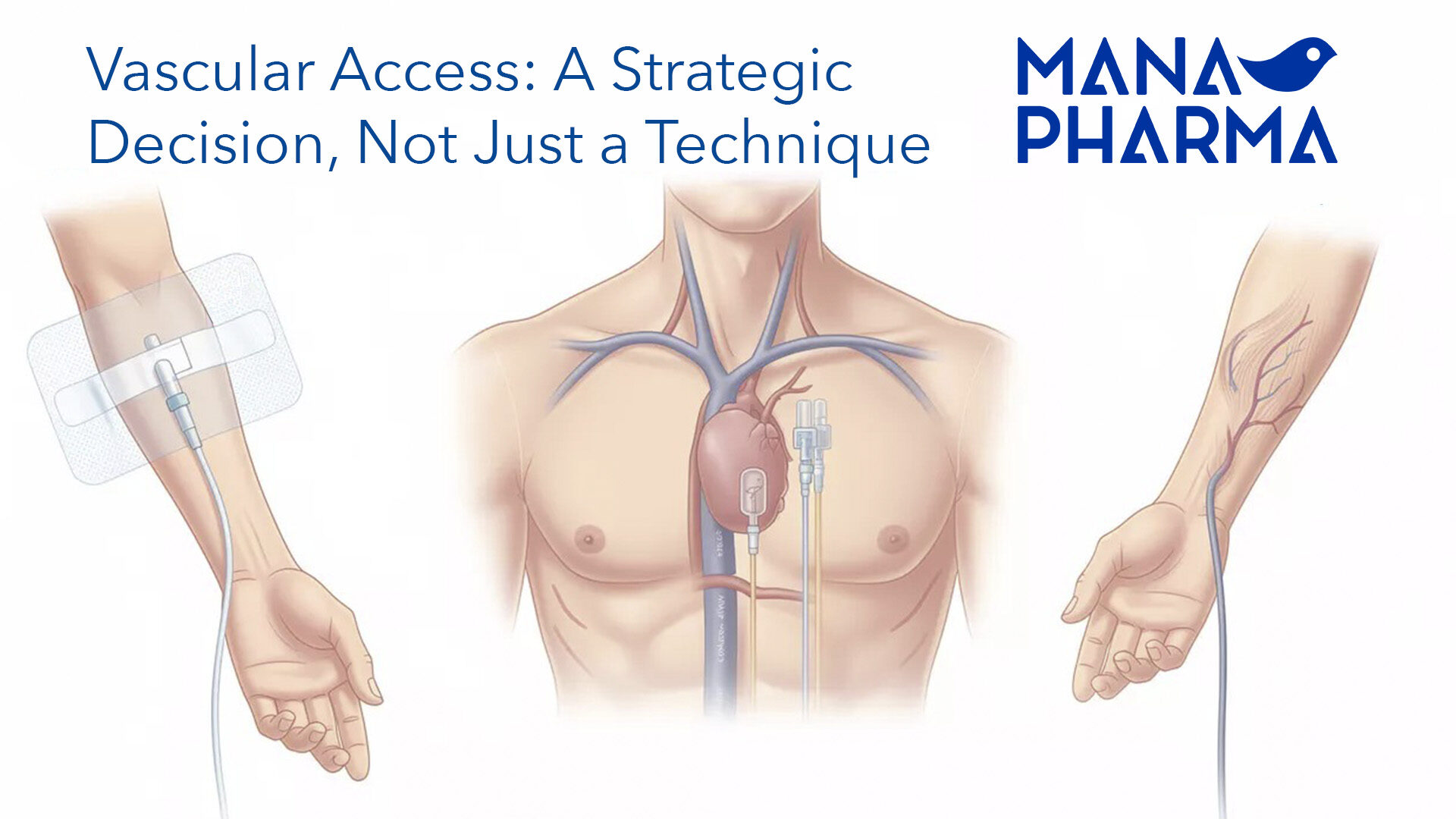
Thrombotic Obstruction in Hemodialysis Catheters: Urgent Evidence for Vascular Nursing
Thrombotic dysfunction in hemodialysis catheters represents a significant burden in clinical practice. A recent systematic review reports that the incidence of thrombosis in hemodialysis catheters ranges from 12% to 52%, depending on follow-up duration and clinical context.
From a pathophysiological perspective, the classic triad of endothelial injury + turbulent flow/stasis + hypercoagulable state is amplified in the catheter setting: biofilm formation, catheter material, and interdialytic stasis promote fibrin deposition and thrombus formation.
Nursing-oriented diagnosis:
Verify that blood flow (Qb) meets minimum standards and observe free backflow without resistance.
Exclude kinking, clamping, or catheter malposition (possible after patient repositioning).
Check connections, clamps, catheter pathway, and possible precipitates/proteins that may compromise the catheter lumen.
If suspicion persists after these steps, request diagnostic imaging (Doppler ultrasound) to rule out thrombosis.
Warning signs requiring escalation:
Sudden pain or edema in the limb with the catheter.
Fever without another evident source or signs of sepsis.
Complete inability to aspirate or infuse through the catheter.
Key readings:
López-Rubio M, et al. “A Comprehensive Review of Catheter-Related Thrombosis.” J Clin Med. 2024;13(24):7818.
Smit JM, et al. “Incidence of catheter-related thrombosis and its determinants in critically ill patients.” Thrombosis Research. 2024; S0049-3848(24)00200-7.