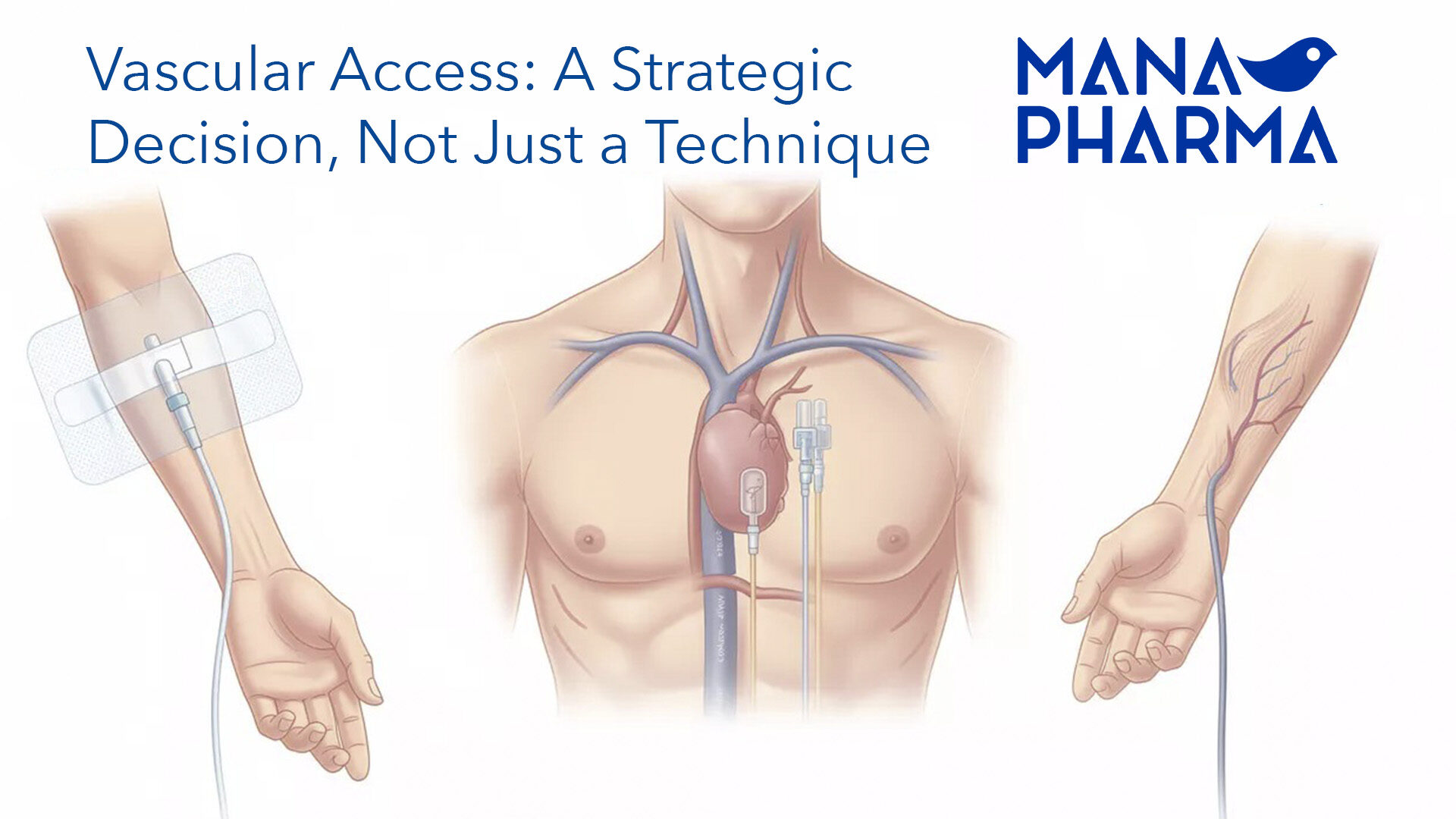
Vascular Access: When the Decision Must Be Strategic, Not Just Technical
In daily clinical practice, a significant proportion of adverse events related to vascular access do not stem from the puncture technique itself, but from an inadequate choice of device from the outset. Incorrect catheter size, underestimation of treatment duration, or an incomplete assessment of the patient’s clinical context frequently lead to preventable complications.
Choosing a vascular access device should not be an automatic or rigidly protocolized decision. On the contrary, it requires a strategic approach based on treatment duration, the type of medication, and the patient’s individual profile.
Three critical decisions from the start
1. Actual duration of treatment
Accurate time forecasting is essential. A treatment lasting fewer than five days is not the same as one extending from five to fourteen days, or beyond two weeks. Each scenario calls for a different optimal device, both in terms of safety and efficiency.
2. Type of medication to be administered
Drug characteristics directly determine the most appropriate vascular access. Medications with extreme pH, high osmolarity, vesicant properties, or biological therapies are not always safe via peripheral access. The idea that “anything goes” is not supported by the evidence.
3. Patient profile
Venous fragility, comorbidities, infection risk, and the potential future need for additional vascular access must all be part of the initial assessment. A poor decision today may compromise therapeutic options tomorrow.
An evidence-based practical rule
👉 An inappropriate access chosen today is almost a guaranteed complication tomorrow.
Optimizing vascular access selection helps reduce phlebitis, catheter-related infections, unnecessary replacements, healthcare costs, and workload. This is not a minor technical detail, but a key component of patient safety and quality of care.
Recommended reading
Chopra V et al. The Michigan Appropriateness Guide for Intravenous Catheters (MAGIC).
Annals of Internal Medicine, 2015.